Abstract
Background: Patients with cancer have an increased risk of venous thromboembolism (VTE) requiring anticoagulation, as well as an increased risk of thrombocytopenia due to cancer therapies or cancer itself. The optimal management of patients with VTE and thrombocytopenia is unclear.
Objective: We performed a systematic review and meta-analysis to evaluate the rates of recurrent VTE and major bleeding in patients with cancer associated thrombosis and thrombocytopenia according to different anticoagulation management strategies.
Methods: We searched MEDLINE, Embase, Scopus, and Cochrane Central Register of Controlled Trials from inception to February 5, 2022. Studies assessing adult patients with cancer associated thrombosis and thrombocytopenia (platelet count < 100 x 109/L) due to malignancy or cancer therapy were included. Three main anticoagulation management strategies were reported: full dose (therapeutic dose anticoagulation +/- platelet transfusion support), modified dose (including 50% dose, prophylactic dose, or shortened duration of anticoagulation), or no anticoagulant. The primary efficacy outcome was recurrent VTE, and the primary safety outcome was major bleeding as defined by individual studies. Secondary outcomes included clinically relevant non-major bleeding, total bleeding events, and all-cause mortality. By using R software (version 4.0.3), the incidence rates of thrombotic and bleeding outcomes by anticoagulation management strategies were pooled using random effects model and expressed as events per 100 patient-months with associated 95% confidence intervals (CI). The quality of studies was assessed by ROBINS-I tool.
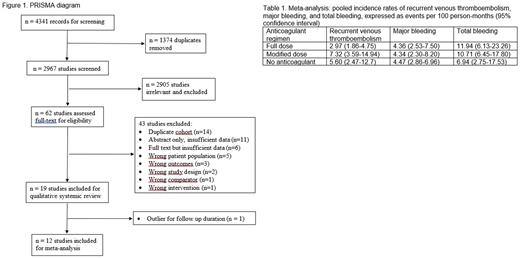
Results: After screening 4,341 records, we included 19 studies (N=1,728 patients with platelet count < 100 x 109/L) in the systematic review, 12 of which were included in the meta-analysis (N=790) (Figure 1). There were no RCTs, two prospective cohort studies, and the rest were retrospective cohort studies. Most studies were small (N=13-471) and limited to patients with platelet count < 50 x 109/L. The majority (~90%) of patients had hematological malignancies or stem cell transplant. Low-molecular-weight heparin was the main anticoagulant reported. All studies were judged to have serious risk of bias, mainly from bias due to confounding and bias due to deviations from intended interventions.
The rates of recurrent VTE, major bleeding, and total bleeding events stratified by anticoagulation management strategies (full dose, modified dose, no anticoagulation) were summarized in Table 1. The rates of recurrent VTE and bleeding complications were high regardless of the management strategies - recurrent VTE on full dose anticoagulant: 2.97 per 100 patient-months (95% confidence interval [CI] 1.86-4.75), modified dose: 7.32 per 100 patient-months (95% CI 3.59-14.94); major bleeding on full dose: 4.36 per 100 patient-months (95% CI 2.53-7.50), modified dose: 4.34 per 100 patient-months (2.30-8.20) (Table 1). There was high degree of heterogeneity in the patient population included, acuity and type of VTE, bleeding criteria used, and follow-up durations. Most studies did not account for the differences in baseline characteristics when outcomes associated with different anticoagulation strategies were reported and analyzed, which could influence the results.
Conclusions: Patients with cancer associated thrombosis and thrombocytopenia have high risks of both recurrent VTE and major bleeding. Our systematic review and meta-analysis demonstrated significant heterogeneity in study conduct and reporting. Our ability to draw a firm conclusion to guide management from the current literature is severely hindered by this limitation. RCTs are needed to define the optimal care for this high-risk population.
Disclosures
Wang:Valeo: Other: Advisory board; Servier: Other: Advisory board; Leo Pharma: Research Funding. Carrier:Pfizer: Consultancy, Honoraria, Research Funding; Bayer: Consultancy, Honoraria; BMS: Consultancy, Honoraria, Research Funding; Servier: Consultancy, Honoraria; Sanofi: Consultancy; Leo Pharma: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.